Overview
The Anesthesiology Critical Care Medicine Fellowship is an ACGME-accredited, year-long training program providing comprehensive, multidisciplinary education in adult critical care medicine, currently approved for three positions per year. Our program aims to prepare fellows to be exceptionally well-trained intensive care specialists, to become diplomates of the American Board of Anesthesiology and Critical Care Medicine, and to develop into future leaders in the field of critical care medicine.
Our program is based on the NewYork-Presbyterian/Weill Cornell Medical Center campus on the Upper East Side of Manhattan, overlooking the scenic East River. The hospital, previously named The New York Hospital, was founded in 1771 and is one of the oldest in the nation. It formed a partnership with the medical school of Cornell University in 1913 and has been based on the Upper East Side since 1932. NewYork-Presbyterian/Weill Cornell Medical Center is a tertiary/quaternary care center, level I trauma center, primary stroke center, and houses the William Randolph Hearst Burn Center and the Ronald O. Perelman Heart Institute. Weill Cornell also boasts affiliations with nearby Rockefeller University, Memorial Sloan Kettering Cancer Center, and the Hospital for Special Surgery.
Fellowship Program
Clinical Experience
The critical care fellowship strongly emphasizes cross-department collaboration and learning, with an emphasis on developing skills in cardiothoracic surgical critical care. Our fellows benefit from our robust academic and busy clinical environments, yet the intimate size of the program allows for customization of a personalized learning plan.
Our fellows spend their year training in the institution’s various intensive care units, including the cardiothoracic ICU, surgical ICU, medical ICU, and neurosciences ICU. Elective rotation experience is available in the (medical) cardiac ICU, pediatric ICU, and mixed medical-surgical ICU at Memorial Sloan Kettering. Each of these experiences provides exposure to unique patient populations and disease processes.
Core Rotations
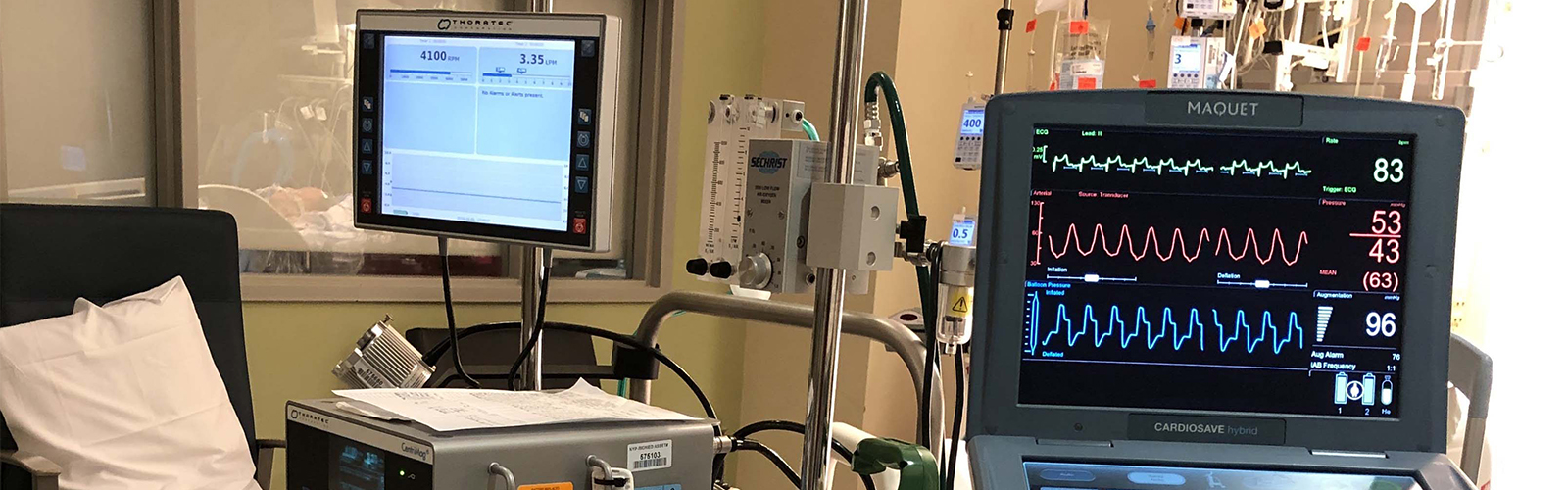
Cardiothoracic ICU
We have a long-standing collaboration with the Department of Cardiothoracic Surgery in primarily managing the cardiothoracic surgical ICU (CTICU), a 20-bed ICU caring for complex, comorbid cardiac and thoracic surgery patients. Fellows play an instrumental role in the perioperative management of patients after CABG, multiple-valve repairs or replacements, major aortic aneurysm or dissection repairs, open thoracoabdominal aortic aneurysm repairs, ventricular assist devices (VADs) insertion or replacement, veno-venous or veno-arterial extracorporeal membrane oxygenation (ECMO), heart transplant, robotic cardiac surgeries, pneumonectomy and esophagectomy, among others. Fellows develop comfort working in a fast-paced, dynamic clinical environment, and gain competencies in numerous ICU procedures, including thoracentesis, synchronized cardioversion, insertion of transvenous pacemakers, awake bronchoscopy, in addition to vascular access procedures such as arterial lines, central lines, and non-tunneled dialysis access.
Surgical ICU
In the SICU fellows manage patients in organ and multisystem organ failure after trauma, massive burn injuries, liver and kidney transplants, major general, colorectal, vascular, or urologic surgeries, and high-risk obstetric patients. Weill Cornell is an American College of Surgeons-designated Level I adult and Level II pediatric trauma center, as well as home to the William Randolph Hearst Burn Center, which is world-renowned for its expertise in burn management.
Medical ICU
In the medical ICU (MICU), fellows gain broad knowledge in the management of a wide scope of critical medical conditions. This includes the management of patients with acute and chronic lung diseases, gastrointestinal diseases, endocrine disorders, hematologic disorders, and organ or multisystem organ failure from malignancy. Furthermore, fellows gain appreciation of differences in the management of critically ill medical patients and critically ill surgical patients.
Neurosciences ICU
While rotating through the neurosciences ICU, fellows acquire knowledge of the management of critically ill patients with neurological or neurosurgical diseases and emergencies. As Weill Cornell is a primary stroke center, fellows will help manage patients with acute strokes. Fellows also learn the interpretation of EEGs, help manage patients with acute seizure disorders, patients after intracranial tumor resections, major spine surgeries, cerebral embolization procedures, head trauma, and other neurosurgical procedures. During this rotation fellows also gain experience with targeted temperature management and the determination of brain death.
Elective Rotations
Pediatric ICU
The pediatric ICU (PICU) at NewYork-Presbyterian/Weill Cornell is part of the NewYork-Presbyterian Komansky Children's Hospital. This elective rotation allows fellows to gain a deeper understanding of pediatric critical illness, and the unique use of various life support modalities in this patient population, such as high-frequency oscillatory ventilation and ECMO.
MSKCC ICU
The Memorial Sloan Kettering elective ICU rotation allows our fellows to take care of critically-ill cancer patients in an advanced specialized cancer center. Many patients that fellows encounter during this elective rotation have advanced, refractory disease, and are undergoing novel and experimental treatments at the forefront of the field.
Other Electives
In addition to critical care exposure, fellows in our program will also rotate in several other subspecialties to create a well-rounded knowledge base. Electives are flexible, and our faculty work with the fellows to personalize a schedule that tailors to each fellow's needs and interests. Previous fellows have chosen to pursue electives in infectious disease, nephrology, echocardiography, heart failure cardiology, and radiology, and previous fellows have taken the initiative to set up international rotations as well.
Fellowship Tracks Overview
While the primary emphasis of critical care fellowship is on the development of superb clinical fellows, we recognize that most fellows also hold academic and professional development aspirations that gravitate toward specific areas. Our optional fellowship track system seeks to promote fellows’ growth in these other areas of focus, with the goal for the year’s additional experience to act as a springboard for their early attending career. Fellows choose a track at the beginning of the academic year and will be mentored throughout the year by an experienced faculty member recognized in that field.
Our fellowship tracks are divided into:
- Clinical Research Track
- Perioperative Critical Care Medicine Leadership Track
- Educational Leadership Track
Clinical Research Track Curriculum
Clinical Research Track fellows will be supervised by faculty mentor Dr. Hannah Wunsch, Professor of Anesthesiology, Vice Chair of Research, and Director of Outcomes Research. Dr. Wunsch is an internationally-renowned scholar in critical care epidemiology. She conducts research and has published extensively on critical care organization and management, utilization of large databases to understand resource utilization, and long-term outcomes of critically ill patients.
Fellows will focus on developing knowledge and skills in:
- Critical review of salient research studies.
- Formation of study hypotheses.
- Development of study protocols.
- IRB approval processes.
- Primary data collection and/or analysis of existing local or national databases.
- Interpretation of data results.
- Development and refinement of analytical and presentation skills.
- Preparation of abstracts and other scholarly work for presentation and publication.
- Formation of mentorship relationships with faculty subject experts.
Fellows on this track will, under the supervision of Dr. Wunsch, receive mentorship from relevant senior faculty, have regular individual check-ins as well as formal quarterly group meetings to discuss proposals, ongoing research/scholar projects and professional development.
In addition, research track fellows will form relationships with internal and external collaborators with an emphasis on work with the potential for national poster and podium presentations, publications, and networking opportunities.
Perioperative Critical Care Medicine Leadership Track Curriculum

Perioperative Critical Care Medicine Leadership Track fellows will be mentored by Dr. Natalia Ivascu Girardi, Professor of Clinical Anesthesiology, Executive Vice Chair for Clinical Affairs, and Division Chief of Critical Care Anesthesiology, and Dr. Sheida Tabaie, Assistant Chief of Critical Care Anesthesiology and Medical Director of the PACU. Dr. Girardi is fellowship-trained in critical care medicine as well as adult cardiac anesthesiology. Dr. Girardi has unique experience and expertise on the delivery of perioperative care. In addition to being the director of the Cardiothoracic ICU, she has been director of liver transplant anesthesiology and as well as director of the Preanesthesia Evaluation Center. Both Drs. Girardi and Tabaie have lectured nationally and internationally on various areas in critical care and perioperative care.
The goals of the leadership fellowship track are aimed at honing one’s leadership skills through critical evaluation of one’s strengths and weaknesses and learning about different leadership skills through both reading/discussion and participating directly in leadership experiences within our hospital system. Throughout the fellowship, enrolled fellows will engage in a variety of activities, including:
- Personality test – identifying strengths and weaknesses; identify leadership style
- Public speaking – how to write and deliver a talk
- Leading a team/communication styles/psychological safety
- Giving feedback
- Conflict resolution/negotiation
- Mentoring and professional networking
- CV writing
- Organizational management and scheduling
- Joining multidisciplinary leadership meetings related to Cardiogenic Shock, ECMO, Inter-ICU, and SCCT (Subcommittee on Critical Care Therapeutics).
Throughout the year, fellows on this track will acquire knowledge and develop skills that will be practiced and refined in the multidisciplinary ICU environment. This track is designed for motivated fellows aspiring to become medical directors and/or hospital administrators. The capstone project is the creation of a Statement of Key Contributions, which involves crafting future goals and mapping out a strategic pathway to achieve these goals.
Educational Leadership Track
Educational Leadership Track fellows will be mentored by Dr. Julia Sobol, a nationally recognized educational leader. The year is focused toward building a more in-depth understanding of program improvement and program development principles relevant to critical care training. Fellows on this track will have the opportunity to collaborate with departmental, Center for Perioperative Outcomes (CPO) and clinical research leaders on designing and conducting their projects. This innovative fellow track is designed to assist fellows to develop knowledge and skills necessary for a successful post-graduate career in educational leadership.
The goals of this track include:
- Acquisition of knowledge and advanced skills in an educational area of interest (Simulation, innovative educational tools, POCUS education, etc.)
- Participation in program improvement and development.
- Enhanced understanding and knowledge of evidenced-based best teaching practices.
- Educational research.
- Development of educational leadership skills.
Academic Activities, Opportunities, and Support
For all fellows, regardless of chosen track, the fellowship features a wide array of didactic teaching sessions spread throughout the year.
When fellows begin their year from July through August, we help speed their transition to our units with a series of boot-camp lectures – focused on high-yield topics given by attending experts of their respective fields, such as ECMO by our ECMO medical director, VADs by a heart failure cardiologist, blood management by our blood bank director, and others. Many of these talks are shared with our junior cardiothoracic surgery fellows, which helps build early camaraderie and familiarity.
Each month, we hold several recurring educational activities. Attending-led didactics are lectures given by attendings in their areas of expertise; with a wide range of topics, from sepsis, to cardiac output monitoring, to pulmonary hypertension. Journal club is led by a fellow with a faculty mentor, and scrutinizes recent, salient studies, or previously accepted landmark trials in critical care. Challenging case discussion is also led by a fellow with attending mentorship, and presents a recent difficult case for discussion among our division. These sessions are usually highly educational and very clinically germane. Board review starts early in the academic year to prime fellows for studying, reinforcing concepts for the critical care board exam. Multidisciplinary critical care conference is held in collaboration with the divisions of Pulmonary Critical Care, Surgery Critical Care, Neurocritical Care, and Pediatric Critical Care – each month one division delivers a lecture on a topic relevant to all intensivists and invites discussions on different management styles and perspectives. POCUS reading sessions reinforce POCUS image acquisition skills and optimization techniques.
Our program strongly encourages echocardiography and critical care point-of-care ultrasound (POCUS) education. Our POCUS curriculum includes a series of lectures given throughout the year, and our credentialed faculty regularly leads POCUS image reading sessions to provide our fellows with constant feedback and skill refinement. Fellows have the opportunity to gain necessary knowledge and skills while preparing for the CCEeXAM by the National Board of Echocardiography, and to meet training requirements for certification in Special Competency in Critical Care Echocardiography. Fellows can also choose to take an elective rotation in perioperative TEE and build enough experience towards Basic PTEeXAM certification in perioperative transesophageal echocardiography.
The fellows in our program participate in several large multidisciplinary simulations throughout the year with cardiothoracic surgeons, CTICU nurses, physician assistants, and nurse practitioners. These simulations focus on life-threatening emergencies in the CTICU and emphasize both the medical decision-making as well as team-work dynamics that result in success for the patient.
A number of “all-fellow” didactics and seminars are held throughout the year. Organized by the Anesthesiology Department, fellows of all anesthesiology subspecialties are encouraged to attend. These sessions include discussions on physician wellness, financial literacy, cultural competency, healthcare disparities, quality improvement methodology, clinical research design, and communications skills. Practice OSCEs and mock oral board exams are also held annually, open to all anesthesiology fellows who are eligible for these exams.
Our vibrant academic atmosphere provides ample opportunity for fellows to be involved in scholarly activities and quality improvement projects during their year. All fellows are expected to participate in a quality improvement project throughout their training, in which they will be heavily involved in the planning and implementation of improvements and enhancements to current patient care practices. Additionally, fellows are also expected to produce scholarly work during their year. In past years fellows have been involved in writing book chapters, case presentations at departmental grand rounds, multidisciplinary institutional conferences, and case presentations at national anesthesiology or critical care conferences. All fellows have the opportunity to participate in clinical outcomes or trials research, which has resulted in abstract publications in previous years.
Early in the year, fellows are each asked to choose a faculty mentor who can help guide their growth throughout their training, giving advice and acting as a sounding board for managing challenges. Our department also provides resources for professional coaching, and interested or motivated fellows are encouraged to participate to help propel their early career.
Critical care fellows receive academic support through a variety of means. At the beginning of the year, all fellows receive two critical care textbooks published by the Society of Critical Care Medicine - Comprehensive Critical Care: Adult, to serve as a comprehensive review book; and Self-Assessment Adult Multiprofessional Critical Care, which contains questions and answers to aid in board exam studying. Fellows receive an academic stipend to be used towards other academically or professionally related expenses. All fellows are strongly encouraged to present at national conferences and receive financial support for these travel and conference-related expenses. Our fellows have a dedicated office space for academic and clinical work and relaxing and receive generous meal cards as well as department provided weekday dinner.
Fellowship Structure
The year of fellowship is divided into core rotations and electives.
Core rotations include:
- Cardiothoracic surgical ICU (CTICU) - 4 months
- Surgical ICU (SICU) - 3 months
- Medical ICU (MICU) - 1 month
- Neurosciences ICU (Neuro ICU) - 1 month
Electives are flexible and may include:
- Pediatric ICU
- Memorial Sloan Kettering ICU
- Transesophageal echocardiography (TEE)
- Echocardiogram reading
- Body imaging radiology
- Critical care nephrology
- Critical care infectious disease
- Heart failure cardiology
- Clinical research
- Quality improvement
Other electives are possible, and we encourage our fellows to tailor their elective experience to maximally benefit their education.
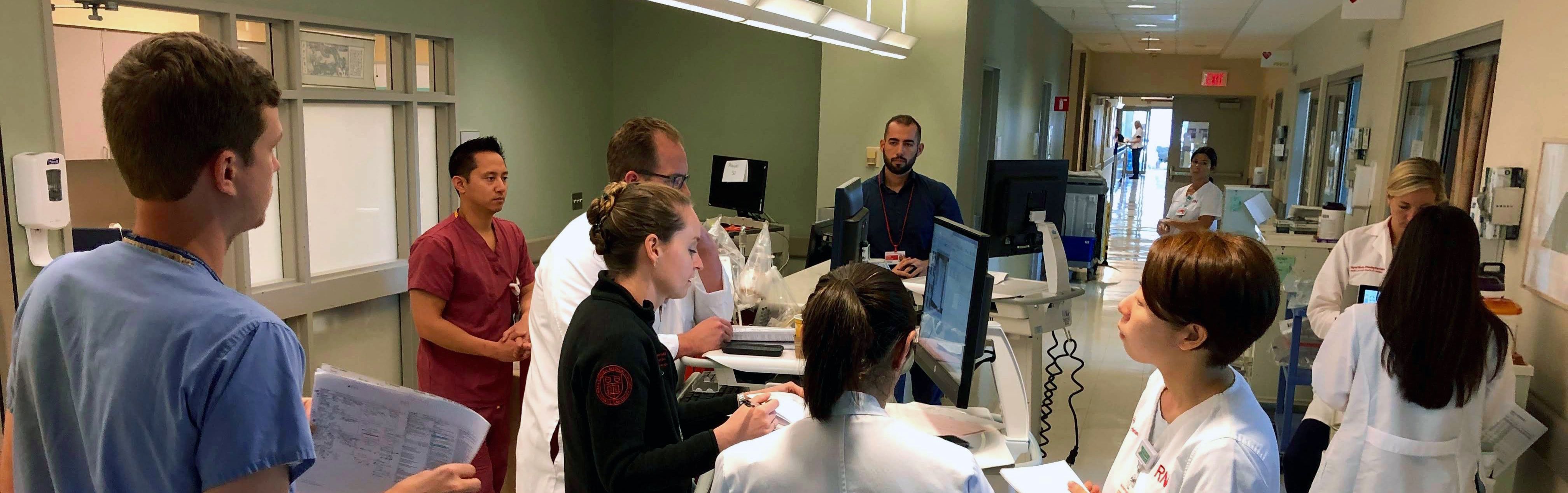
During rotations in the CTICU and SICU, the fellow on-service will be the primary fellow taking care of the patients in the ICU. PAs and residents are expected to primarily “carry” patients, with responsibilities including order-entry and note handoff updates, while the fellow is expected to supervise this work and engage in diagnosis and treatment option considerations. With guidance from the on-service attending, the fellow will evaluate and treat all patients admitted on the unit, while providing instruction, teaching, and supervision to the residents and physician assistants (PAs) in the unit. The fellow role is to apply critical-thinking and diagnosis skills to our critically ill patients and ensure timely, appropriate care of those patients, and to take increasing responsibility in directing the multidisciplinary team, which includes anesthesiology and surgery residents, PAs, respiratory therapists, dieticians, pharmacists, and physical therapists.
We strictly maintain training structure within ACGME guidelines and New York State law for managing fellow workload, including work hours, mandatory time off, access to call rooms, and recourse if fellows are unable to provide care for any reason. All fellows take 4 weeks of vacation per year, and attempts are made to maximize flexibility for scheduling time off. Our fellows take part in institutional as well as departmental wellness initiatives, which include division happy hours, multidivision outings, and others. While the critical care fellowship year is a busy one, our program, department, and institution are supportive of wellness-related needs of our fellows.
How to Apply
Eligibility:
To be eligible to apply, fellowship applicants must have successfully completed four years of training in an anesthesiology ACGME-accredited residency program in the United States. In accordance with the hospital's GME policy, we are currently only considering applicants with J1 visas.
Dual Critical Care Medicine/Cardiothoracic Anesthesia Fellowships:
Special consideration will be made for applicants who are interested in completing our Critical Care Medicine and Cardiothoracic Anesthesiology fellowships in sequence. Candidates interested in being considered for acceptance to both programs should submit their formal application using on SFMatch.
Application Process:
Our program participates in the online San Francisco (SF) Match (sfmatch.org), which uses the Central Application Service (CAS) to collect and distribute application materials during the match process.
Applicants must first register with SF Match and submit their initial application materials using CAS and upload the following documents:
CAS application form on SF Match website. (Please include a photo and personal statement)
- Three letters of reference, one of which must be from the applicant’s residency program director
- Curriculum Vitae
- USMLE (steps 1-3) or NBME (1-3) score reports
- Most recent anesthesiology in-training exam (ITE) or board exam scores (BASIC exam, etc.)
Anesthesiology Critical Care Fellowship contact: Marlene Augustine
maa2010@med.cornell.edu
Applications are reviewed in full and interview invitations are offered and conducted on a rolling basis.
Fellowship positions for the 2027-2028 academic year will have the following timeline:
- Application registration begins: November 10, 2025 on sfmatch.org
- Interviews will be offered and conducted on a rolling basis: January - March
- Rank list due on SF Match: May 28, 2026
- Match results are released: June 4, 2026
- Fellowship start date: July 1, 2027
Fellowship Leadership

Julia Sobol, MD, MPH
Program Director, Anesthesiology Critical Care Medicine Fellowship
Associate Professor of Clinical Anesthesiology
Contact:
Marlene Augustine, Fellowship Program Coordinator
Phone: (212)746-2785
E-mail: maa2010@med.cornell.edu
Current Fellows

Kirk Benack, MD, PharmD
2025-2026
Kirk Benack was born and raised in Pennsylvania. He completed a Pharm.D. at the Ernest Mario School of Pharmacy and subsequently obtained an M.D. from Robert Wood Johnson Medical School through Pharm.D./M.D. dual-degree program. He completed his residency training at Montefiore Medical Center and served as chief resident.

Boris Borovcanin, MD, MA
2025-2026
Dr. Borovcanin grew up in Buffalo, New York. He earned a Bachelor of Arts in biology from the University of Rochester and a Master of Arts in physiology from the Jacobs School of Medicine and Biomedical Sciences at the University at Buffalo. As an undergraduate, he was awarded the URMC Summer Scholars Program Research Grant for work investigating cardiac ischemia-reperfusion injury and cardioprotection. Dr. Borovcanin received his M.D. from Jagiellonian University Medical College in Kraków, Poland, and completed his anesthesiology residency at the University at Buffalo.
Alice Qin, MD
2025-2026
Dr. Alice Qin received her undergraduate degree from the University of Rochester, after which she conducted research in pediatric oncology at Johns Hopkins prior to attending medical school at New York Medical College. She subsequently completed residency in anesthesiology at the University of Maryland.
Former Fellows 2024-2025

Federico Ciardi, MBBS
2024-2025

Daniel Schwartz, MD
2024-2025
Former Fellows

Nicolas Govea, MD
2023-2024

Linjia Jia, MD
2023-2024

Rebecca Piland, MD
2023-2024
Michael Chang, MD
2022-2023

Austin Meszaros, MD
2022-2023

Shamik Patel, MD
2022-2023

Maria Betances Fernandez, MD
2021-2022

Anastasia Meleties, MD
2021-2022

Klint Smart, MD
2021-2022
Sho Tanaka, MD
2020-2021

Sana Na Javeed, MD
2019-2020

Alexandra Rhee, MD
2019-2020

Samir Sethi, MD
2019-2020

Caryl Bailey, MD
2018-2019

Rebecca Lee, MD
2018-2019

Ankur Srivastava, MD
2018-2019

Krish Sekar, MD
2016-2017

Michael Katz, MD
2016-2017

Michael Andrews, MD
2015-2016

Joshua Kohtz, MD
2015-2016

Gurbinder Singh, DO
2015-2016
Sheida Tabaie, MD
2014-2015
Christopher Tam, MD
2014-2015

Yan Yuhong, MD
2014-2015